Medicare Part B Penalties and SEPs
Compare Medicare Plans & Costs
Run a quick Medicare comparison, then request help confirming the best next step for your Part B timing.
Prefer to talk? Call 800-533-5969
Get Help Avoiding Part B Penalties
Confirm SEP eligibility, document employer coverage, and choose the best Part B start date with a quick review.
Request Help (Penalty & SEP Review) Medicare Services Call 800-533-5969
Medicare Part B penalties and SEPs can feel confusing because the rules include multiple enrollment windows, different types of employer coverage, and paperwork requirements that vary depending on your situation. The good news is that the penalty triggers are predictable. Once you know what Medicare considers “creditable” for delaying Part B — and how Special Enrollment Periods (SEPs) work — you can avoid permanent premium surcharges and enroll on the correct timeline with confidence.
This guide breaks down the Part B late enrollment penalty, explains when SEPs apply (and when they do not), and gives practical “real world” examples for common scenarios. If you are still working past 65, covered under a spouse’s employer plan, moving from employer coverage to Medicare, or trying to coordinate retirement timing with Medicare and Social Security, this is the page you want to read carefully.
Avoid Medicare Part B Penalties
Check timing, confirm SEP eligibility, and prevent permanent premium surcharges.
What is the Part B late enrollment penalty?
The Medicare Part B late enrollment penalty is an additional premium surcharge that can be added to your Part B monthly premium if you delay enrollment when you were supposed to enroll — and you do not have a valid, Medicare-recognized reason for delaying. The key point is that Medicare does not care whether you were “healthy” or “didn’t need doctor coverage.” If you were eligible and did not enroll, Medicare looks only at whether you had qualifying coverage that allowed you to delay.
The most common valid reason for delaying Part B is being covered by active employer group health coverage (yours or your spouse’s) from current employment. In many cases, if the employer is large enough and the coverage is considered appropriate for delaying Part B, Medicare allows you to enroll later using a Special Enrollment Period and avoid penalties.
When penalties apply, they can be painful because they are usually long-lasting. Instead of a one-time fee, the penalty typically increases your ongoing Part B premium in a way that remains in place as long as you have Part B. That is why getting the timing right matters so much.
How the Part B penalty is calculated
The Part B penalty is calculated using a simple concept: Medicare looks at how long you went without Part B coverage after you should have had it, and it adds a percentage surcharge to your premium. The common rule of thumb is this: for each full 12-month period you could have had Part B but did not enroll, Medicare may add a 10% surcharge to your Part B premium.
That surcharge is generally tied to the standard premium calculation framework Medicare uses. Even if premiums change over time, the percentage penalty can follow you forward, which is why a “small delay” can turn into a large lifetime cost depending on your age and how long you remain enrolled.
Here’s what this means in practical terms: if someone delays Part B for multiple full years with no qualifying employer group coverage, they may be paying a higher Part B premium permanently. This is why people who are unsure should not guess. They should confirm their eligibility to delay, confirm Medicare primary/secondary rules, and document coverage before making a timing decision.
Part B SEPs: who qualifies and how the window works
A Special Enrollment Period (SEP) for Part B is Medicare’s way of allowing a penalty-free enrollment after age 65 when you delayed Part B because you were legitimately covered by active employer group health coverage. The SEP exists to protect working individuals (and in many cases spouses) who are covered through current employment and do not need Part B immediately.
The SEP window is often described as an 8-month window that begins when employment ends or employer coverage ends, whichever happens first. The practical takeaway is that you do not want to wait. Retirement, layoffs, job changes, and HR delays can create paperwork problems. The best time to gather documentation is before your employment or employer coverage ends, not after.
Another practical point: many people confuse “having insurance” with “having qualifying insurance.” Medicare is specific about what counts for Part B SEP purposes. Employer coverage tied to active employment is usually the key. If coverage is not tied to active employment, Medicare may not view it the same way.
Employer coverage rules: when Medicare is primary vs secondary
One of the biggest reasons Part B penalty mistakes happen is that people assume employer coverage always makes delaying Part B safe. In reality, the relationship between Medicare and employer coverage depends on the employer size and plan coordination rules. The question that matters is: who pays first — Medicare or the employer plan?
In many situations with a larger employer group plan, the employer coverage may remain primary and Medicare may be secondary. In those cases, delaying Part B may be reasonable, but it must be confirmed. In other situations — especially smaller employer plans — Medicare may be primary. If you delay Part B when Medicare is supposed to be primary, you may run into claim denials or costly out-of-pocket exposure, and the delay may also trigger a penalty later.
This is why we recommend confirming the employer size and coordination rules with HR in writing. Do not rely on assumptions or verbal statements. If you are coordinating Medicare timing with Social Security, it also helps to understand the broader system interaction: how Medicare and Social Security work together.
If you’re still working past 65 and unsure what to do, this guide provides a practical framework: How to Get Medicare While Working.
Timelines, forms, and documentation (avoid delays)
Using an SEP for Part B is often straightforward — until paperwork slows things down. Medicare and Social Security typically require proof of employer coverage after age 65. The documentation confirms that you were covered by a qualifying employer group plan tied to active employment and that you are eligible to enroll penalty-free.
Two forms are commonly referenced in SEP enrollment situations. One is the application to enroll in Part B, and the other is the request for employment information that your employer completes. The important practical point is that employer HR departments can be slow, and mistakes on these forms can cause processing delays. If you know you’re approaching retirement, start this process early.
If you want a broader Medicare overview so this decision fits your entire coverage plan, you can also review the Medicare structure here: Medicare Services.
COBRA, retiree plans, Marketplace, and other special situations
Special situations are where Part B penalty mistakes are most common. Many people believe COBRA coverage is “employer coverage,” so it must allow them to delay Part B. That assumption can be costly. COBRA often begins after active employment ends, and Medicare may not treat COBRA the same way as active employer coverage for SEP purposes.
Retiree coverage can create similar confusion. Retiree plans may be valuable, but they are often not the same as active employer group coverage from current employment. Marketplace (ACA) plans also frequently cause confusion, because they are legitimate health insurance — but they typically do not create a Part B SEP.
Because Medicare decisions can have permanent cost consequences, this is where professional review matters. If you are transitioning from employer coverage, COBRA, or a retiree plan, it’s smart to confirm the best Part B start date before you cancel anything.
Realistic examples by situation
Example 1: Working past 65 at a large employer. A person turns 65, stays employed, and keeps employer group coverage. They confirm in writing that the employer plan remains primary. They delay Part B and later enroll during the SEP after retirement. When done correctly, this can allow a penalty-free Part B enrollment and a smooth transition to Medicare.
Example 2: Retiree chooses COBRA and delays Part B. A person retires, elects COBRA, and assumes Part B can be delayed. If Medicare does not treat COBRA as qualifying for an SEP, they may be late enrolling into Part B, risking penalties and coverage gaps. The safer path is usually to confirm Part B timing before leaving employment and not rely on COBRA assumptions.
Example 3: Small employer plan past 65. Someone works for a smaller employer and stays on the employer plan. If Medicare is expected to be primary, delaying Part B can create claim issues. In these situations, enrolling at 65 is often the safer approach, but the correct answer depends on plan coordination rules that should be confirmed with HR.
Example 4: Spouse coverage. A spouse remains actively employed with qualifying employer group coverage, and the Medicare-eligible spouse stays on the plan. In many cases this can allow a penalty-free delay, but it should be verified and documented. This is one of the most common SEP pathways that works well when handled properly.
IRMAA vs penalties: timing choices that matter
It’s important not to confuse IRMAA with late enrollment penalties. IRMAA is a premium adjustment based on income, while the Part B penalty is based on being late without a valid reason. A person can avoid penalties and still face IRMAA if income is high. Similarly, a person can have modest income and still face a penalty if Part B enrollment was delayed incorrectly.
That said, timing still matters. Retirement income events can cause premium changes later, so Medicare decisions should be made with a full view of retirement timing, income planning, and coverage structure. If you are coordinating Medicare enrollment with retirement and Social Security timing, it can help to understand the broader interaction: how Medicare and Social Security work together.
Common mistakes to avoid
The most common Part B mistakes are not “careless.” They happen because people assume coverage rules are intuitive. They are not. The safest approach is to confirm your specific situation and document it in writing.
Common mistakes include assuming COBRA creates a Part B SEP, assuming retiree plans work like active employer coverage, missing SEP windows after employment ends, failing to confirm employer size, and waiting until claims are denied before fixing enrollment timing. If you are uncertain, review options with a Medicare advisor before making changes.
Get help with Medicare Part B penalties and SEPs
If you’re unsure whether you can delay Part B or whether your employer coverage qualifies for an SEP, we can help you confirm eligibility, identify what documentation you need, and choose a Part B start date that avoids penalties and protects your coverage.
Start with a quick request and we’ll guide you from there. You can also review our Medicare guidance hub here: Medicare Services.
Want a Part B Timing Review?
We’ll confirm if employer coverage qualifies, document your SEP, and help prevent permanent premium penalties.
Related Medicare Pages
Keep learning and compare your options with these Medicare guides.
Compare Medicare Carriers
Book a free consultation with Tonia to review highly-rated Medicare Advantage plans and choose the best fit for your retirement.
FAQs: Medicare Part B penalties and SEPs
What triggers the Medicare Part B late-enrollment penalty?
You can be penalized if you delay Part B past your Initial Enrollment Period and you don’t have qualifying active employer group coverage (yours or a spouse’s) that allows a Special Enrollment Period.
How much is the Part B penalty and how long does it last?
The penalty is generally 10% of the standard Part B premium for every full 12-month period you delayed without a qualifying reason, and it typically lasts as long as you have Part B.
What is a Special Enrollment Period (SEP) for Part B?
A Part B SEP is a window that lets you enroll in Part B without a penalty when you delayed because you had active employer group coverage after 65 and then that job or coverage ended.
Does COBRA or retiree coverage qualify me for a Part B SEP?
Usually no—COBRA and retiree coverage are not treated as active employment for Part B SEPs, so delaying Part B on COBRA alone can lead to penalties.
How long is the Part B SEP window?
The Part B SEP is generally available for at least 8 months after the earlier of when employment ends or when the employer coverage ends, so it’s best to start paperwork before coverage stops.
What forms do I usually need to enroll during a Part B SEP?
Commonly requested forms include CMS-40B (Part B enrollment) and CMS-L564 (employer verification of coverage), with the employer completing the L564.
Does employer size matter if I’m still working at 65?
Yes—if your employer has fewer than 20 employees, Medicare is often primary, and delaying Part B may cause claim issues and penalties, so confirm payer rules with HR in writing.
Can a Part B penalty be removed once it’s applied?
Most Part B penalties are effectively permanent while you have Part B, though rare exceptions may apply if you can document misinformation or qualifying circumstances through a formal review process.
About the Author:
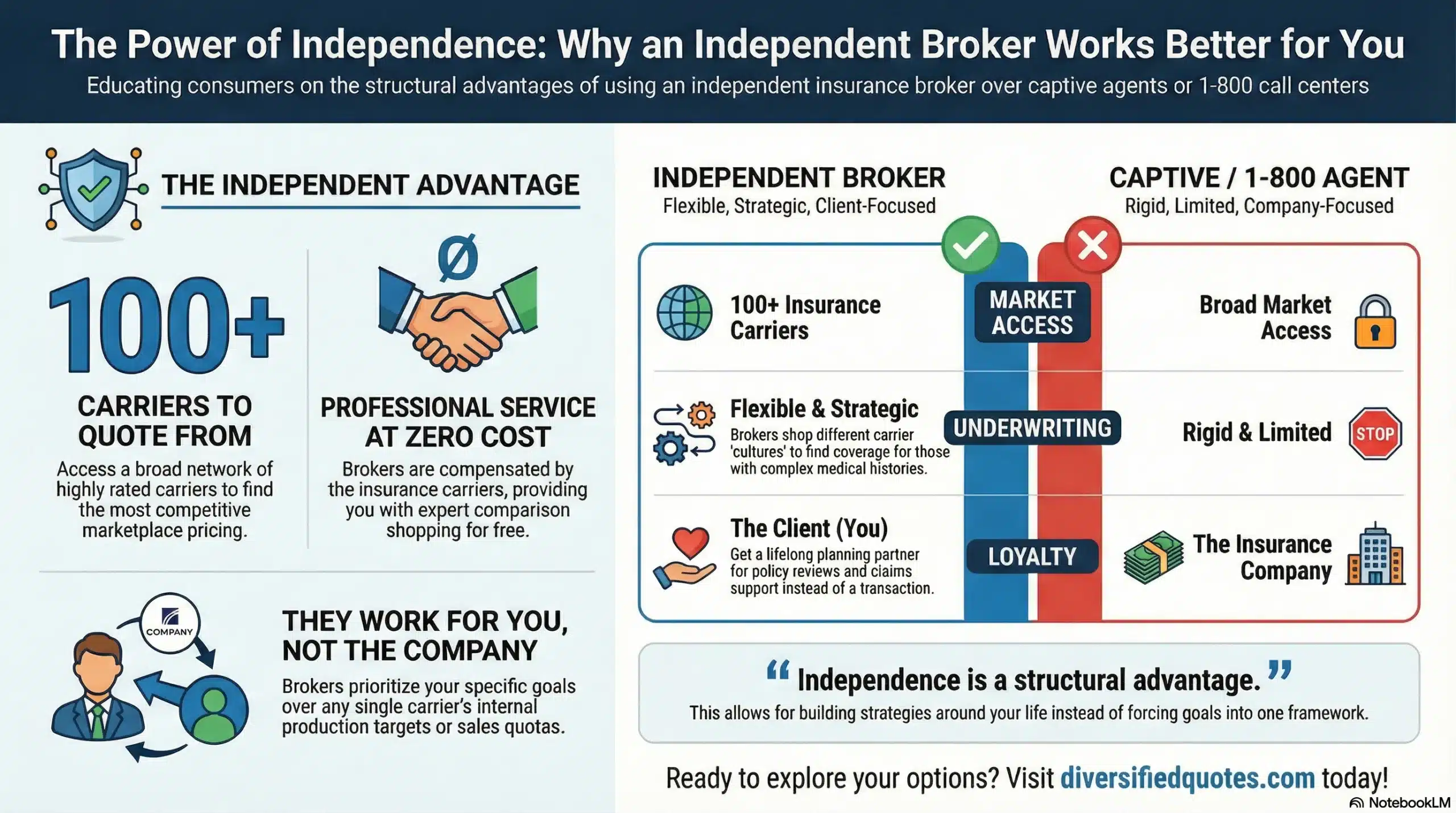
Tonia Pettitt, CMIP©, is a seasoned Medicare specialist with more than 40 years of hands-on experience guiding individuals and families through the complexities of Medicare planning. As a senior advisor with the nationally licensed independent agency Diversified Insurance Brokers, Tonia provides clear, dependable guidance across all areas of Medicare—including Medicare Advantage, Medicare Supplement (Medigap), and Part D prescription coverage. Leveraging active contracts with dozens of highly rated insurance carriers, she helps clients compare options objectively and secure the most suitable coverage for their health and budget.
Known for her patient, education-first approach, Tonia has built a reputation as a trusted resource for retirees seeking reliable, unbiased Medicare support. With four decades of experience across evolving Medicare laws, carrier changes, and plan structures, she brings unmatched insight to every client conversation—ensuring clients feel confident, protected, and fully prepared for each stage of their retirement healthcare journey.
