Medicare Enrollment Mistakes to Avoid
Avoid Costly Medicare Enrollment Mistakes
A missed deadline or the wrong plan choice can trigger penalties, delays, and expensive surprises. Get help confirming the right steps for your situation.
Request Medicare Enrollment HelpEstimate Your Medicare Plan Costs
Use this tool to compare Medicare plan structures and costs. It’s a helpful starting point before you confirm networks, prescriptions, and enrollment timing.
Medicare enrollment mistakes to avoid can save you thousands of dollars and prevent coverage headaches that linger for years. Medicare is not difficult because it is “complicated math.” It is difficult because the rules depend on timing, on what type of coverage you already have, and on what you are trying to accomplish (Original Medicare + supplement, Medicare Advantage, prescription coverage, or a combination). A small misunderstanding at the start can create penalties, gaps, or limited choices later.
At Diversified Insurance Brokers, we guide Medicare clients nationwide through enrollment so they can avoid the most common and costly errors. People often assume Medicare works like group health insurance where you pick a plan once and forget about it. In reality, Medicare has multiple parts, multiple enrollment windows, and multiple rules that interact with employer coverage, COBRA, retiree coverage, HSAs, and prescription drug timing. The goal is not just to “enroll,” but to enroll in the right way for your specific situation.
One reason mistakes happen is that Medicare enrollment is often triggered during life transitions. People are retiring, switching jobs, moving states, helping a spouse, or dealing with a new diagnosis. When you are focused on big life decisions, paperwork deadlines can be easy to overlook. Unfortunately, Medicare deadlines can have permanent effects, especially for Part B and Part D penalties. That is why the best strategy is to treat enrollment as a planning event, not an administrative task.
The most common and expensive mistake is misunderstanding the timing around your Initial Enrollment Period (IEP). Your IEP is generally a seven-month window around your 65th birthday month. If you do not have qualifying coverage and you delay, you can be hit with late-enrollment penalties and may also have to wait for the next available enrollment period to get coverage activated. The cost of “waiting” is not only the penalty — it can be the gap and the stress of not having coverage when you need it.
Another major mistake is assuming you can delay Part B because you have some type of coverage that “feels” like insurance. Medicare has specific rules about which coverage allows you to delay Part B without penalty. Active employer group coverage often qualifies when the employer size rules are met, but COBRA and many retiree plans do not protect you from Part B penalties the way people expect. This mistake is especially common for retirees who accept COBRA thinking it is a bridge, then later discover Medicare rules treat that bridge differently.
For people who want Original Medicare plus a Medicare supplement (Medigap), the next major pitfall is missing the best enrollment window for Medigap. Many retirees do not realize there is a valuable period tied to your Part B effective date where Medigap access is typically easiest and most predictable. If you miss that opportunity, you may face underwriting later depending on state rules and your health history. That is why the “order of operations” matters: timing Part B correctly can protect your ability to buy the supplement strategy you want.
Medicare Advantage plan selection creates a different category of mistakes. Advantage plans are popular because they bundle coverage and may offer additional benefits. But they are not one-size-fits-all. A common error is enrolling without confirming provider networks. If your primary doctor, specialist, hospital system, or clinic is not in-network, your access and costs can change immediately. For people with ongoing care needs, network alignment is not optional — it is the foundation of whether the plan works in real life.
Prescription coverage adds another layer. Many retirees underestimate how important Part D or integrated drug coverage can be. Choosing a plan with the wrong formulary or tiering can create large out-of-pocket costs during the year, even if the monthly premium looks attractive. The “best” drug plan is not the cheapest premium — it is the plan that produces the lowest total annual cost for your medication list and preferred pharmacy, while keeping access stable.
Another mistake we see is assuming that a “$0 premium” Medicare Advantage plan means healthcare will be inexpensive. A zero premium plan can still have meaningful copays, coinsurance, and authorization rules that add up quickly, especially if you use care frequently. The plan might still be a good fit — but only after reviewing the full cost structure, the out-of-pocket maximum, and the network. A premium is only one part of total cost.
People also overlook how much plans change from year to year. Networks shift. Formularies shift. Benefits shift. Even if you enrolled correctly the first time, you can still be impacted by changes later. This is why annual reviews are important. The goal is to catch changes early and adjust during the enrollment period, rather than discovering a problem after the year begins.
Enrollment mistakes can also affect spouses differently. One spouse may be on Medicare while the other is not yet eligible. The decisions you make about employer coverage, retiree coverage, COBRA, and timing can affect both of you. This is another reason personalized help matters — the “simple” answer often ignores real household complexity.
Finally, Medicare planning should include the reality of how you use healthcare. People who rarely see doctors may prioritize premium savings. People who use specialists, imaging, therapies, or ongoing prescriptions may prioritize stability and lower cost sharing. The biggest mistake is choosing a plan based on generic advice rather than your actual usage and your actual providers.
Not Sure Which Enrollment Window Applies to You?
We’ll help you confirm the right timing and the right plan structure so you avoid penalties, delays, and coverage gaps.
Get Enrollment GuidanceTo avoid mistakes, the best approach is to treat Medicare enrollment as a checklist. First, confirm whether you should enroll at 65 or delay based on qualifying employer coverage. Second, choose your preferred plan structure: Original Medicare with a supplement, or Medicare Advantage. Third, confirm prescription coverage that aligns with your medications and pharmacies. Fourth, confirm provider access so the plan works with your doctors and facilities. Finally, schedule annual reviews so you can respond to plan changes before they become problems.
When people follow this process, they dramatically reduce the chance of penalties, surprises, and lost options. Medicare becomes less stressful because decisions are made on purpose. The goal is a plan that fits your medical needs, your budget, and your preferred way of accessing care.
If you’d like help avoiding Medicare enrollment mistakes, we can walk you through the correct timing and plan selection steps for your ZIP code. We’ll help you compare options clearly so you can enroll with confidence.
Let’s Avoid Costly Medicare Mistakes Together
Submit your details and we’ll confirm enrollment timing, plan structure, provider access, and prescription coverage.
Start Your Medicare Enrollment ReviewRelated Medicare Pages
Keep learning with these Medicare enrollment and plan selection guides.
Medicare for People with Chronic Conditions Medicare Part B Penalties and Special Enrollment Periods How to Choose the Best Medicare Plan Medicare Plans with Dental and Vision Coverage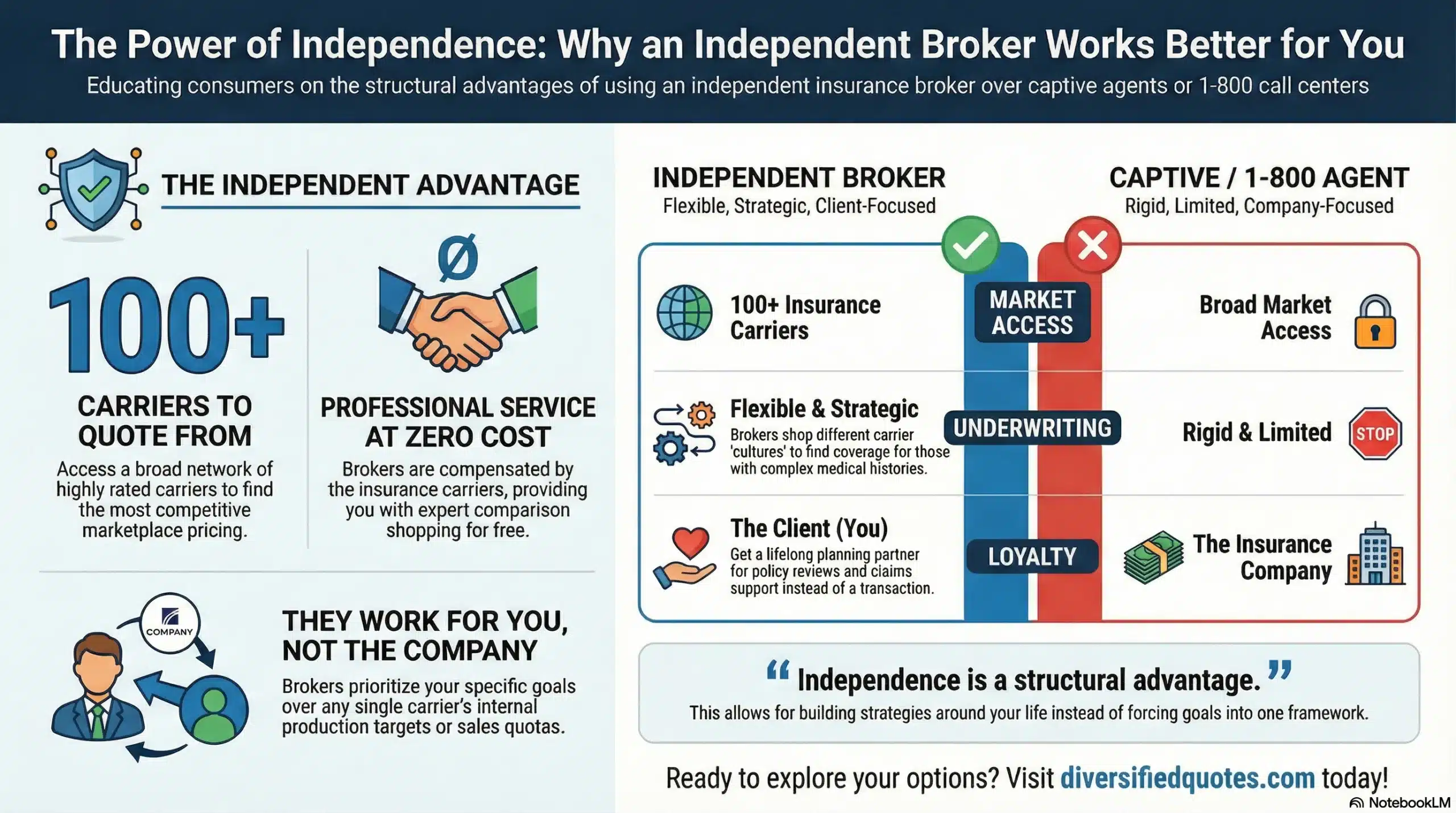
Compare Medicare Carriers
Book a free consultation with Tonia to review highly-rated Medicare Advantage plans and choose the best fit for your retirement.
FAQs: Medicare Enrollment Mistakes to Avoid
What’s the most common Medicare enrollment mistake?
Missing your Initial Enrollment Period (IEP) without qualifying coverage. Delays can lead to penalties and gaps in coverage timing.
When is my Initial Enrollment Period (IEP)?
It’s generally a 7-month window: the 3 months before your 65th birthday month, your birthday month, and the 3 months after.
Can I delay Part B without a penalty if I’m still working?
Often yes, if you have qualifying active employer group coverage. The details depend on your situation and how the coverage is structured.
Is COBRA or retiree coverage “creditable” for delaying Part B?
Many people are surprised here. COBRA and retiree coverage often do not protect you from Part B penalties the way active employer group coverage does. Confirm your situation before delaying.
What about Part D late-enrollment penalties?
If you go without creditable prescription coverage beyond an allowed window, you may face a Part D penalty. Continuous creditable drug coverage is the safest approach.
How does employer size affect enrolling at 65?
Employer size can influence whether Medicare is primary or secondary. This can affect whether delaying Part B is appropriate and whether penalties apply.
Can I keep contributing to an HSA after I start Medicare?
No. Once Medicare coverage begins, HSA contributions generally must stop. Planning timing is important if you are still contributing.
Should I verify doctors and prescriptions before choosing a plan?
Yes. Confirm providers and facilities for Medicare Advantage networks and confirm your medications and pharmacies for prescription coverage.
Do I need to review my Medicare coverage every year?
Yes. Networks, formularies, and benefits can change annually. Reviewing during enrollment periods helps prevent surprises.
About the Author:
Tonia Pettitt, CMIP©, is a seasoned Medicare specialist with more than 40 years of hands-on experience guiding individuals and families through the complexities of Medicare planning. As a senior advisor with the nationally licensed independent agency Diversified Insurance Brokers, Tonia provides clear, dependable guidance across all areas of Medicare—including Medicare Advantage, Medicare Supplement (Medigap), and Part D prescription coverage. Leveraging active contracts with dozens of highly rated insurance carriers, she helps clients compare options objectively and secure the most suitable coverage for their health and budget.
Known for her patient, education-first approach, Tonia has built a reputation as a trusted resource for retirees seeking reliable, unbiased Medicare support. With four decades of experience across evolving Medicare laws, carrier changes, and plan structures, she brings unmatched insight to every client conversation—ensuring clients feel confident, protected, and fully prepared for each stage of their retirement healthcare journey.
